Pneumonia: Stop It Before It Starts – Risk & Protection Guide
Pneumonia is not listed as a separate disease in the global top 10. Instead, it falls under the broader category of Lower Respiratory Infections (LRIs). Notably, LRIs, which include pneumonia, rank as the 4th leading cause of death worldwide and affect millions each year. Importantly, pneumonia does not strike at random. Rather, it carefully targets vulnerabilities within our bodies and lifestyles. In doing so, it exploits these weaknesses to establish a devastating infection deep in the delicate air sacs of the lungs.
Therefore, by understanding this targeting mechanism, we can build strong defenses. As a result, this allows us to move from potential victims to vigilant guardians of our respiratory health. Furthermore, this guide goes beyond the basic symptoms. It not only breaks down the blueprint of pneumonia risk but also gives you the knowledge to stop this illness before it starts.
In this post, we will explore Pneumonia Risk and Proactive Protection.
The Unseen Battle Within: How Pneumonia Exploits Our Weaknesses?
Pneumonia begins when microbes—bacteria, viruses, or fungi—bypass the body’s natural defenses. This triggers a severe inflammatory response inside the alveoli. The alveoli are tiny air sacs in the lungs that are essential for oxygen exchange. When infected, they fill with fluid and pus. This leads to the classic symptoms of pneumonia: coughing, fever, and severe breathlessness.
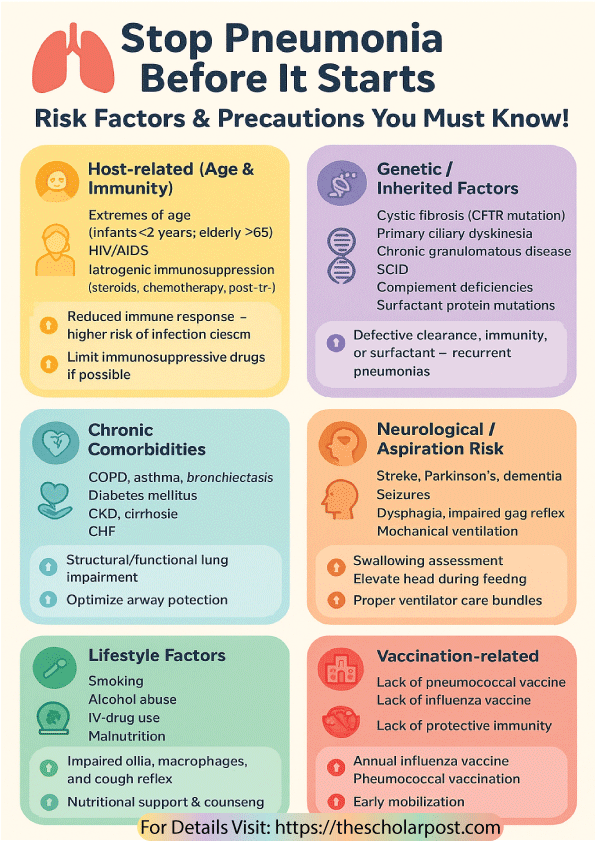
Every risk factor for pneumonia is linked to a breakdown in these defenses. This breakdown may involve immune suppression, structural damage, or increased exposure to harmful pathogens. The details of these risk factors are summarized in Table 1.
Risk Factors for Pneumonia
| Table 1: Risk Factors for Pneumonia | ||
| Category | Specific Risk Factors | Pathophysiological Basis |
| Host-related (Age & Immunity) | – Extremes of age (infants <2, elderly >65) – HIV/AIDS – Iatrogenic immunosuppression (corticosteroids, chemotherapy, post-transplant) | Reduced cellular and humoral immune response predisposes to infection by encapsulated and opportunistic pathogens |
| Genetic / Inherited Factors | – Cystic fibrosis (CFTR mutation) – Primary ciliary dyskinesia (Kartagener’s syndrome) – Chronic granulomatous disease (NADPH oxidase defect) – Severe combined immunodeficiency (SCID) – Complement deficiencies (C3, C5–C9) – Surfactant protein gene mutations | Impaired mucociliary clearance, defective phagocytosis, impaired antibody/complement function, or abnormal surfactant metabolism lead to recurrent bacterial/viral pneumonias |
| Chronic Comorbidities | – COPD, asthma, bronchiectasis – Diabetes mellitus – CKD, cirrhosis – Congestive heart failure | Structural lung damage, impaired mucociliary clearance, altered neutrophil/lymphocyte function |
| Neurological / Aspiration Risk | – Stroke, Parkinson’s disease, dementia – Seizures – Dysphagia, impaired gag reflex – Mechanical ventilation | Loss of airway protection → aspiration of oropharyngeal/gastric secretions |
| Lifestyle Factors | – Smoking – Alcohol use disorder – IV drug use – Malnutrition | Smoking damages cilia and macrophages; alcohol alters flora and cough reflex |
| Environmental / Exposure | – Crowded living (prisons, nursing homes) – Pollutants, occupational dust/fumes – Viral epidemics (influenza, RSV) | Facilitates pathogen transmission and epithelial injury, predisposing to superinfection |
| Healthcare-associated | – Recent hospitalization (>48 hrs) – ICU admission – Invasive devices (ET tube, catheters) – Prolonged immobility | Colonization by multidrug-resistant organisms (Pseudomonas, MRSA) |
| Vaccination-related | – Lack of pneumococcal vaccination – Lack of influenza vaccination | Failure to mount protective immunity against respiratory pathogens |
Host-related pneumonia risk
Extremes of age represent one of the most significant and unavoidable risk factors for developing severe pneumonia, primarily due to the distinct immunological challenges presented by both infancy and advanced age. Infants younger than two years possess an immune system that remains naïve and underdeveloped, lacking prior exposure to a wide array of pathogens and therefore unable to mount a robust, targeted defense against invading organisms. Conversely, adults over the age of sixty-five experience immunosenescence, a gradual deterioration of the immune system that diminishes both the potency and efficiency of its response, effectively leaving the lungs vulnerable to infection. Furthermore, conditions like HIV/AIDS or iatrogenic immunosuppression from chemotherapy, corticosteroids, or post-transplant medications deliberately suppress immune function, creating a wide-open pathway for opportunistic pathogens to cause infection.
Precautions and preventive measures for these groups must be exceptionally robust and meticulously followed, focusing primarily on vaccination as a first line of defense. Annual influenza shots and pneumococcal vaccines (both PCV15/PCV20 and PPSV23) are non-negotiable pillars of prevention, significantly reducing the incidence and severity of pneumonia. For individuals with HIV, strict adherence to antiretroviral therapy (ART) is paramount for restoring immune function, while physicians should regularly review the necessity and dosage of any immunosuppressive drugs to minimize risk.
Genetic predisposition to pneumonia
A small but significant portion of the population inherits a genetic predisposition to recurrent respiratory infections through various rare but impactful disorders. Cystic fibrosis, caused by a mutation in the CFTR gene, creates abnormally thick mucus that traps bacteria instead of allowing the body to clear it, thereby turning the airways into a fertile breeding ground for infection. Similarly, primary ciliary dyskinesia involves defective cilia—the microscopic hair-like structures that sweep debris from the airways—resulting in stagnant mucus and recurrent pneumonias. Other conditions, like chronic granulomatous disease, severe combined immunodeficiency (SCID), and complement deficiencies, cripple the immune system’s ability to kill ingested bacteria and fungi, leaving the body utterly defenseless against common microbes.
Precautions and preventive measures for these individuals require a highly specialized and multidisciplinary medical approach. Genetic counseling provides families with essential information about inheritance patterns and future risks, while daily chest physiotherapy (postural drainage) is critical for mechanically clearing the tenacious mucus from the lungs. Many patients rely on long-term prophylactic antibiotics to suppress bacterial growth, and groundbreaking interventions like stem cell or gene therapy now offer potential cures or long-term management strategies for specific conditions like SCID.
The Domino Effect: How Chronic Diseases Amplify Pneumonia Risk
Pre-existing chronic medical conditions act as powerful amplifiers for pneumonia risk by compromising the structural integrity and functional capacity of the lungs and other vital organs. Chronic obstructive pulmonary disease (COPD) and asthma cause persistent inflammation and airway obstruction, while bronchiectasis permanently damages the airway walls, impairing mucus clearance and creating pockets for infection. Systemic diseases like diabetes mellitus elevate blood sugar levels, which inadvertently suppresses immune function and enhances the virulence of certain bacteria; meanwhile, chronic kidney disease, cirrhosis, and congestive heart failure (CHF) promote fluid overload and edema, including within the lungs, creating an ideal environment for bacterial growth.
Precautions and preventive measures hinge on the aggressive and optimal management of the underlying comorbidity itself. Consistently controlling blood sugar in diabetics, managing fluid balance in CHF patients, and adhering to prescribed inhalers for COPD and asthma drastically reduce baseline vulnerability. Pulmonary rehabilitation programs can remarkably improve lung strength and endurance, and patients must adopt a policy of seeking early treatment at the very first sign of any respiratory infection to prevent a minor issue from escalating into full-blown pneumonia.
The Silent Threat: Neurological Conditions and Aspiration Pneumonia
Aspiration pneumonia is a unique and dangerous condition. The threat does not come from the external environment. Instead, it comes from within the body. It happens when oral or gastric contents are inhaled into the lungs. Neurological conditions such as stroke, Parkinson’s disease, and dementia increase the risk. These conditions impair the delicate neuromuscular coordination needed for safe swallowing, a problem known as dysphagia. They also weaken the protective gag reflex. Seizures can cause a sudden loss of consciousness. During this time, vomiting and aspiration may occur.
Critically ill patients on mechanical ventilation face additional risks. Their airway is breached by the ventilator. This makes them highly vulnerable to ventilator-associated pneumonia (VAP).
Precautions and preventive measures for aspiration risk are intensely practical and focus on mechanical protection. A formal swallowing assessment is essential for diagnosing dysphagia. This assessment is usually performed by a speech-language pathologist. It helps identify safe swallowing techniques and appropriate food textures.During feeding, individuals should always remain in an upright position. The head should be elevated to at least 30 degrees. Caregivers must also provide thorough and regular oral care to reduce the bacterial load in the mouth.
In hospitals, strict adherence to ventilator care bundles is critical. These bundles include elevating the head of the bed and providing regular oral care with chlorhexidine. Such practices have been proven to drastically reduce the rates of ventilator-associated pneumonia (VAP).
Lifestyle and Environment: The Modifiable Risks Within Your Control
Among the most empowering categories of risk factors are those related to lifestyle and environment because they are almost entirely modifiable through conscious choice and behavioral change. Smoking paralyzes the cilia that clear mucus from the airways, destroys lung tissue, and cripples the macrophages that patrol the alveoli for invaders. Alcohol abuse sedates the very same protective cough and gag reflexes that prevent aspiration, while intravenous drug use increases the risk of septic emboli that can travel to the lungs. Malnutrition, particularly protein-energy deficiency, starves the immune system of the essential building blocks it requires to manufacture antibodies and immune cells, leading to a profoundly weakened defense system.
Precautions and preventive measures here are clear and unequivocal: smoking cessation stands as the single most effective action any individual can take to improve their respiratory health and reduce pneumonia risk. Reducing alcohol consumption to moderate levels or eliminating it entirely removes a significant suppressor of vital reflexes, and seeking professional support for substance abuse is critical. Nutritional support and counseling can reverse the immunosuppressive effects of malnutrition, ensuring the body has the fuel it needs to fight off infections.
Healthcare-associated pneumonia
Ironically, the very places we seek healing can also carry hidden dangers. Hospitals and long-term care facilities are major sources of multidrug-resistant organisms (MDROs) such as MRSA and Pseudomonas aeruginosa. Recent hospitalization, ICU stays, major surgery, and prolonged immobility all raise the risk of bacterial colonization. These potent bacteria can invade the lungs if given an opportunity, such as through a ventilator tube or during a period of weakened immunity.
Precautions and preventive measures for HAP and VAP are the cornerstone of modern hospital infection control protocols. Meticulous hand hygiene—using alcohol-based rubs or soap and water—for every staff member, patient, and visitor is the undisputed first rule of prevention. Hospitals implement strict infection control practices, including the careful de-escalation of broad-spectrum antibiotics to prevent the development of further resistance. For patients, early mobilization—getting out of bed and moving as soon as it is medically safe—is a simple yet powerfully effective tactic for improving lung expansion and clearing secretions.
The Final Arbiter: The Non-Negotiable Role of Vaccination
The absence of recommended vaccinations is one of the easiest risk factors to correct. In fact, choosing not to vaccinate means giving up a powerful and proven shield against specific pathogens. Fro example, influenza virus infection can cause severe damage to the respiratory lining. As a result, this damage creates an opportunity for secondary bacterial pneumonia to develop. Moreover, streptococcus pneumoniae remains one of the leading bacterial causes of community-acquired pneumonia in all age groups.
Precautions and preventive measures could not be more straightforward: get vaccinated. Specifically, receiving an annual influenza vaccine is the best defense against seasonal flu and its dangerous complications. In addition, pneumococcal vaccination provides direct protection against the most common bacterial strains. According to current CDC guidelines, vaccination is recommended for children, adults over 65, and people with specific risk factors.
Vaccination is safe and effective. It is also a collective responsibility. Not only does it protect the individual, but it also strengthens community herd immunity. In turn, this helps safeguard those who are too vulnerable or too young to be vaccinated.
Ultimately, preventing pneumonia is an active and ongoing process of risk assessment and mitigation. By carefully understanding the specific factors that apply to you or your loved ones, you can engage in a targeted and informed dialogue with your healthcare provider. Through this approach, you can implement a personalized strategy that dramatically reduces the odds of this serious infection. Remember, your lungs are your lifeline—fortify their defenses today.
Top 7 Questions & Answers on Risk Factors of Pneumonia
Which age groups are most vulnerable to pneumonia and why?
Infants below 2 years and elderly individuals above 65 years are at the highest risk. In infants, the immune system is immature, with reduced antibody production and underdeveloped lung defenses. In the elderly, immunosenescence (age-related decline in immunity) combined with chronic illnesses weakens their ability to fight pathogens. This explains why both extremes of age are more prone to severe or recurrent pneumonia.
Name two genetic disorders that increase pneumonia susceptibility.
Genetic conditions like cystic fibrosis and primary ciliary dyskinesia predispose individuals to recurrent respiratory infections. In cystic fibrosis, thickened mucus obstructs airways, providing a fertile ground for bacterial growth. In primary ciliary dyskinesia, defective cilia impair mucociliary clearance, preventing the lungs from efficiently expelling pathogens. These inherited disorders highlight the role of genetics in pneumonia vulnerability.
How does smoking predispose to pneumonia?
Cigarette smoke contains toxins that paralyze and destroy respiratory cilia, reducing their ability to sweep out mucus and microbes. Additionally, smoking impairs alveolar macrophages—the “cleaning cells” of the lungs—making it easier for pathogens like Streptococcus pneumoniae to establish infection. This explains the higher pneumonia rates among smokers compared to non-smokers.
What is the role of chronic diseases like diabetes in pneumonia risk?
Diabetes mellitus disrupts both innate and adaptive immunity. High blood sugar levels impair neutrophil chemotaxis, phagocytosis, and intracellular killing of bacteria. Furthermore, diabetic patients often have comorbid conditions such as kidney disease or vascular compromise, all of which make recovery from pneumonia slower and complications more frequent.
Why are stroke and dementia patients prone to aspiration pneumonia?
Neurological conditions such as stroke, Parkinson’s disease, or dementia impair swallowing reflexes and reduce cough efficiency. This allows oropharyngeal secretions and gastric contents to enter the lower airways, leading to aspiration pneumonia. In patients on mechanical ventilation, the risk is even higher due to bypassing natural airway defenses.
Which vaccinations are most critical in pneumonia prevention?
The two most effective vaccines are the pneumococcal vaccine and the influenza vaccine. Pneumococcal vaccines protect against Streptococcus pneumoniae, the leading cause of bacterial pneumonia, while influenza vaccination reduces viral infections that can predispose to secondary bacterial pneumonia. Universal immunization has significantly reduced pneumonia-related morbidity and mortality.
How can healthcare-associated pneumonia be prevented in hospitals?
Healthcare-associated pneumonia (HAP), particularly ventilator-associated pneumonia, arises due to colonization by multidrug-resistant organisms. Prevention strategies include rigorous hand hygiene, disinfection protocols, elevating the head of the bed to prevent aspiration, limiting unnecessary antibiotic use, and promoting early patient mobilization. Hospitals with strict infection-control programs show a marked reduction in pneumonia cases.
Further Reading/References
- Centers for Disease Control and Prevention. Pneumonia. Retrieved from https://www.cdc.gov/pneumonia/index.html
- World Health Organization. Pneumonia Fact Sheet. Retrieved from https://www.who.int/news-room/fact-sheets/detail/pneumonia. Last accessed 23/08/2025
- American Lung Association. Preventing Pneumonia. Retrieved from https://www.lung.org/lung-health-diseases/lung-disease-lookup/pneumonia/preventing-pneumonia. Last accessed 23/08/2025
- National Heart, Lung, and Blood Institute. Pneumonia. Retrieved from https://www.nhlbi.nih.gov/health/pneumonia. Last accessed 23/08/2025
- Wunderink, R. G., & Waterer, G. W. (2014). Community-acquired pneumonia. The New England journal of medicine, 370(19), 1863. https://doi.org/10.1056/NEJMc1402692
- UpToDate. Patient education: Pneumonia in adults (Beyond the Basics). Retrieved from https://www.uptodate.com/contents/pneumonia-in-adults-beyond-the-basics. Last accessed 23/08/2025