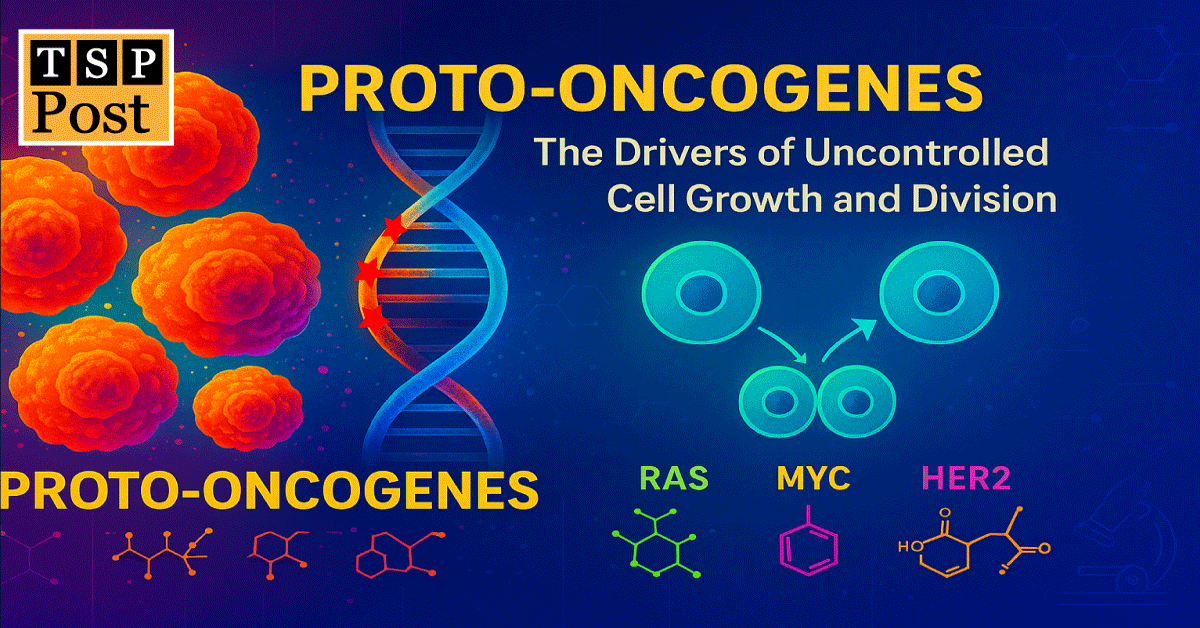
Proto-Oncogenes: The Drivers of Uncontrolled Cell Growth and Division
Introduction: When Growth Signals Go Haywire
In general, cells thrive in a delicately balanced environment, governed by complex genetic instructions. Among these instructions are proto-oncogenes, genes that ensure timely cell growth, differentiation, and repair. But a single mutation can tip the balance. When proto-oncogenes mutate into oncogenes (modified version of proto-oncogenes), they drive unregulated cell proliferation, one of the hallmarks of cancer.
Understanding how these genes function, mutate, and contribute to malignancies is essential for both clinicians and researchers. Therefore, In this article we explore the biology, classification, and clinical implications of proto-oncogenes.
Note: Cancer is a disease of genes. Numerous genes are involved in regulating of cancers. These genes belong to different categories, see our post. “Cancer Genes: The Hidden Drivers Behind Tumor Formation”
What Are Proto-Oncogenes?
When discussing cancer associated genes, particularly proto-oncogenes, the foremost question that arises in our mind is: What are proto-oncogenes? Fundamentally, proto-oncogenes are normal, non-mutated genes present in all cells. They encode proteins that:
- Stimulate cell division
- Transmit growth signals from the cell surface to the nucleus
- Regulate apoptosis (cell death)
- Promote angiogenesis (formation of new blood vessels)
When functioning properly, proto-oncogenes help tissues grow and regenerate. However, if they become mutated, amplified, or dysregulated, they transform into oncogenes that push the cell to divide continuously—regardless of signals or damage.
How Many Proto-Oncogenes Are Known?
Currently, more than 100 proto-oncogenes have been identified in humans. These genes are conserved across species and play crucial roles in embryonic development, immunity, and tissue maintenance. However, only a subset of them—approximately 40–60 proto-oncogenes—are known to be commonly mutated in human cancers.
Classification of Proto-Oncogenes
Proto-oncogenes can be classified based on the functions of their protein products:. Specifically, they fall into the following categories:
- Growth Factors
- To begin with, growth factors are signalling proteins that stimulate cell growth, proliferation, and differentiation by binding to specific receptors on the cell surface.
- They also stimulate cell for initiating specific cellular activity by binding to receptors.
- For example: PDGF (Platelet-Derived Growth Factor)
- Growth Factor Receptors
- Next these receptors receive external growth signals and activate intracellular pathways.
- Notable examples include: EGFR, HER2 (ERBB2)
- Intracellular Signal Transducers
- In addition, these proteins relay signals from receptors to the nucleus.
- Examples include: RAS, ABL, SRC
- Transcription Factors
- Moreover, Transcription factors regulate the expression of genes involved in proliferation.
- key examples are: MYC, JUN, FOS etc.
- Cell Cycle Regulators
- Finally these regulators control progression through the cell cycle.
- Examples include: Cyclin D1 (CCND1), CDK4
This classification is useful in both diagnosing specific cancers and developing targeted treatments.
From Proto-Oncogene to Oncogene: The Dangerous Shift
The transformation of proto-oncogenes into oncogenes occurs via several mechanisms (Table 1):
| Table 1: Mechanisms of Activation: | ||
| Mechanism | Description | Effect on Cells |
| Point Mutation | Single base change alters protein function | Hyperactive or permanently active protein |
| Gene Amplification | Multiple copies of a gene lead to overproduction | Increased protein levels, excessive signaling |
| Chromosomal Translocation | Gene moves to a new location, often under an active promoter | New fusion proteins or overexpression |
| Insertional Mutagenesis | Viral insertion near gene enhances its expression | Overactivation in viral cancers |
Each mechanism removes normal checks and balances, allowing cells to proliferate uncontrollably.
Key Examples of Proto-Oncogenes
Let’s explore some well-known proto-oncogenes and their implications:
- RAS (HRAS, KRAS, NRAS)
- Function: GTPase that transmits growth signals
- Mutation Effect: Constitutive activation → uncontrolled cell division
- Cancers: Pancreatic (90%), colorectal, lung
- MYC (c-MYC, N-MYC, L-MYC)
- Function: Transcription factor that regulates cell cycle and apoptosis
- Mutation Effect: Overexpression leads to unchecked proliferation
- Cancers: Burkitt’s lymphoma, breast cancer, neuroblastoma
- HER2/neu (ERBB2)
- Function: Receptor tyrosine kinase that responds to growth factors
- Mutation Effect: Amplification causes constant signaling
- Cancers: 25–30% of breast cancers (HER2-positive)
- ABL
- Function: Non-receptor tyrosine kinase involved in cell differentiation and division
- Mutation Effect: Fusion with BCR gene → BCR-ABL oncoprotein
- Cancers: Chronic Myeloid Leukemia (CML)
- SRC
- Function: Non-receptor tyrosine kinase involved in cell adhesion and growth
- Cancers: Colon, breast, lung cancers
Proto-Oncogenes vs Tumor Suppressor Genes
Understanding the difference is critical (Table 2):
| Table 2: Contrasting Characteristics of Proto-Oncogenes and Tumor Suppressor Genes | ||
| Feature | Proto-Oncogenes | Tumor Suppressor Genes |
| Primary Role | Actively promote cell growth, division, and survival under normal conditions | Function to inhibit excessive cell growth, repair DNA, or trigger apoptosis |
| Effect of Mutation | Gain-of-function mutations result in constant activation and overactivity | Loss-of-function mutations eliminate protective effects, allowing unchecked growth |
| Cancer Association | Mutation leads to overproliferation and oncogenic transformation | Mutation results in failure to suppress tumors and genomic instability |
| Inheritance Pattern | Typically dominant; mutation in a single allele is enough to influence disease | Generally recessive; both alleles must be inactivated to lose function |
| Examples | RAS, MYC, HER2, ABL | TP53, RB1, BRCA1, APC |
| Therapeutic Implication | Often targeted with inhibitors (e.g., tyrosine kinase inhibitors, monoclonal antibodies) | Restoration or activation of these genes is more challenging, but essential for prevention |
While proto-oncogenes are the “accelerators”, tumor suppressor genes act as “brakes” in the cellular machinery.
Clinical Relevance: Why Should We Care?
Proto-oncogenes have become central targets in modern cancer therapy and diagnostics:
- Diagnostic Significance:
- Clinicians now use mutations in proto-oncogenes as biomarkers.
- Tests like KRAS mutation analysis guide therapy for colorectal cancer.
- HER2 testing determines suitability for trastuzumab therapy.
- Therapeutic Targeting:
- Tyrosine kinase inhibitors (e.g., imatinib for BCR-ABL in CML)
- Monoclonal antibodies (e.g., trastuzumab for HER2)
- RNAi-based gene silencing (experimental stage)
- Personalized Oncology:
- Targeted treatments reduce side effects compared to traditional chemotherapy.
- Next-generation sequencing helps identify multiple proto-oncogene mutations in tumors.
Future Directions: Gene Editing & Precision Oncology
Emerging fields like CRISPR-Cas9 gene editing offer hope to correct proto-oncogene mutations at the DNA level. Additionally:
- Small molecule inhibitors are being designed to target proteins downstream of proto-oncogenes.
- Synthetic lethality approaches target cancer cells that rely on oncogene function while sparing normal cells.
These strategies may someday halt cancer at its genetic roots, offering longer-lasting and more effective treatments.
Conclusion: Small Mutations, Big Consequences
In summary, this post highlights that proto-oncogenes are essential drivers of life—but when misregulated, they become powerful instigators of cancer. Therefore, understanding their functions, classifications, and transformation into oncogenes is key to unlocking targeted, precision-based treatments.
In the evolving landscape of cancer biology, proto-oncogenes represent both a challenge and an opportunity—the perfect illustration of how a cell’s greatest strength can become its greatest vulnerability.
References:
- Weinberg RA. The Biology of Cancer, 2nd Ed. Garland Science.
- Vogelstein B, Kinzler KW. Cancer genes and the pathways they control. Nat Med. 2004.
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011.
- National Cancer Institute. https://www.cancer.gov
- Lodish H. Molecular Cell Biology, 8th Ed. W.H. Freeman.
Frequently Asked Questions and Answers
What are proto-oncogenes and why are they important in cell biology?
This is one of the most commonly asked question. Basically, proto-oncogenes are essential genes found in all normal cells that play a key role in regulating cell growth, differentiation, and survival. In fact, they produce proteins that act as messengers in growth signaling pathways. These genes help cells divide at the right time and stop when necessary. However, if a proto-oncogene mutates or becomes overactive, it can transform into an oncogene, driving continuous cell division. Consequently, this unchecked growth is one of the critical steps in the development of cancer.
What triggers a proto-oncogene to become an oncogene, and what happens next?
A proto-oncogene becomes an oncogene through mechanisms such as point mutations (a single DNA base change), gene amplification (copy number increase), chromosomal translocations (gene rearrangement), or viral insertion. These changes cause the gene to produce too much protein or a protein that is constantly active. As a result, the loss of control over the cell cycle oc, leading to persistent cell division, resistance to death signals, and often, tumor formation.
What are some key proto-oncogenes, their functions, and the cancers they are linked to?
Several proto-oncogenes have been directly associated with specific cancers due to their mutations:
- KRAS: Involved in transmitting growth signals inside the cell; mutated in ~90% of pancreatic cancers, as well as colon and lung cancers.
- MYC: Acts as a transcription factor that controls genes for cell growth and apoptosis; frequently overexpressed in Burkitt’s lymphoma, breast cancer, and neuroblastoma.
- HER2 (ERBB2): A receptor tyrosine kinase; overactive in 25–30% of breast cancers, leading to aggressive tumor growth.
- ABL: A tyrosine kinase that helps regulate cell division; forms a fusion gene (BCR-ABL) in chronic myeloid leukemia (CML).
- SRC: Involved in cell adhesion and growth; abnormally activated in several cancers including colon, breast, and lung.
What distinguishes proto-oncogenes from tumor suppressor genes in cancer biology?
Proto-oncogenes and tumor suppressor genes serve opposite roles in the cell:
| Feature | Proto-Oncogenes | Tumor Suppressor Genes |
| Function | Promote cell growth and division | Inhibit cell division, promote DNA repair or apoptosis |
| Mutation Effect | Gain-of-function (overactivity) | Loss-of-function (inactivity) |
| Mutation Pattern | Dominant (1 allele mutation is enough) | Recessive (both alleles must be mutated) |
| Examples | RAS, MYC, HER2 | TP53, RB1, BRCA1/2 |
Together, these genes maintain cellular balance. When proto-oncogenes are overactive and tumor suppressor genes are lost, it creates the perfect storm for cancer to develop.
Why do proto-oncogenes matter in clinical diagnosis and treatment of cancer?
Proto-oncogenes are at the center of many modern cancer strategies because they serve as biomarkers and therapeutic targets. For example:
- Diagnostic Tests: KRAS mutation testing helps guide treatment decisions in colorectal cancer. HER2 testing in breast cancer determines whether drugs like trastuzumab will be effective.
- Targeted Therapies: Drugs such as imatinib target the BCR-ABL fusion protein in CML. Monoclonal antibodies and small molecule inhibitors are designed to specifically block the activity of oncogenic proteins.
- Precision Medicine: Next-generation sequencing allows oncologists to detect multiple proto-oncogene mutations in tumors, enabling personalized and less toxic treatment plans.
- Future Directions: Approaches like CRISPR gene editing, RNA interference, and synthetic lethality are being explored to disable oncogenes at the genetic level.