The Mystery Behind Several Disorders of Human are Different Types of Abnormal Cells
What are Abnormal Cells?
Before discussing and dissecting our topic “different types of abnormal”, it is compulsory to know about cells. Approximately 30 trillion cells belonging to almost 200 different types (i.e., tissues) collaborate to build the human body. So, there are nearly 200 different types of tissues as well in the human body. The cell is the smallest and basic unit of life. In other words, a cell is the structure and function unit of living things. Body cells perform all characteristic features of living things (i.e., respiration, nutrition, development, movement, reproduction, and sensation. In the case of unicellular organisms, all these cellular activities are performed by single cells. While in the case of multicellular organisms, cells are differentiated into different types after zygote formation. Different types of differentiated cells perform specialized functions. Such type of cellular activities ensures normal life.
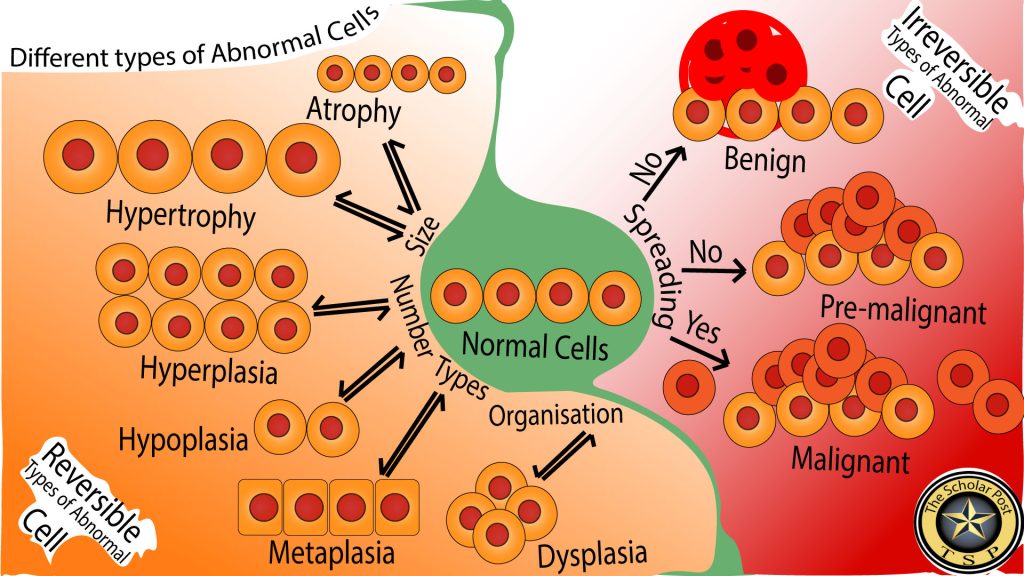
However, due to many reasons (i.e., environmental, genetic, etc.), internal organelles and/or biomolecules can be damaged. Consequently, these cells are unable to perform their assigned functions according to their capability and are stated as Abnormal cells. With advances in life sciences study using advanced technology, it was observed that cellular abnormalities are not similar to each other. Therefore, due to altered function, these cells are divided into different “Types of Abnormal Cells.” This article focuses on different types of abnormal cells (Figure 1: Different types of abnormal Cells.
Classification of Abnormal Cells
Abnormal cells are divided into the following two types based on reversibility properties. Reversible Cell and Irreversible cell.
Reversible Types of Abnormal Cells
When an abnormal cell can be changed back into its normal status such type of cell is known as a reversible cell. Reversible abnormality in cells can be due to an increase or decrease in number, changes in size, location, organization, and/or differentiation. Let’s study briefly different cellular abnormalities based on morphological characters.
Type of Abnormal Cell Based on Size of the Cell
Atrophy
In atrophy, size of the cells decreases due to loss of proteins, organelles, and/or cytoplasmic portion. Cellular shrinkage results in a decrease in tissue size. A well-known example of Atrophy is muscle atrophy (Bonaldo and Sandri, 2013). The cytoplasm of muscle cells consists of contractile proteins. Muscle cells respond differently to two different types of situations, such as in the case of anabolic conditions (healthy activity like exercise) stimulate synthesis of new proteins. These proteins accumulate in the cytoplasmic region, consequently increases the volume of the cell. On the other hand in muscle atrophy, catabolic activities (such as infection, debates, cancer, low activity, or inactivity of organs, etc.) trigger the degradation of proteins in the cytoplasmic region, consequently, shrinkage of volume occurs in the muscle cell. (Sartori et al, 2021).
Hypertrophy
Hypertrophy is the condition in which an increase in the volume of cell size occurred.
Type of Abnormal Cell Based on Number of the Cell
Hyperplasia
It is an increased the number of cells in a tissue. The rate of cell proliferation enhances the cells that escape controlling property of tissue to maintain the quantity of cells. Subsequently, the size of the tissue become enlarged as compared to the normal tissue size of the same cells. Morphologically, these cells look like normal cells.
Causes of Hyperplasia
Several causes (such as infection, compensation of damaged tissue, hormonal dysfunction, stress, disease, etc.) stimulate the hyperplasic condition of a tissue
Hyperplasia Associated Disoders
- Benign Prostatic Hyperplasia (BPH). In BPH, the prostate gland enlarges due to a rise in the number of epithelial and fibromuscular cells located in the transition and periurethral regions (Devlin et al, 2021).
- Lymphoid Liver Hyperplasia. Other names benign nodular lesion and Pseudolymphoma. This disorder has a mass of mature heterogeneous lymphoid cells, lacking noticeable nuclear atypia (Yuan et al, 2012). Lymphocyte-stimulating agents (i.e., infections agents, etc.) result in the proliferation of lymphoid hyperplasia.
- Endometrial Hyperplasia is the consequence of the altered proliferation of the endometrial lining of the uterus, known as endometrium (Nees et al, 2022). The endometrium becomes thick in endometrial hyperplasia.
- Intimal Hyperplasia. Thickening of the intimal layer due to the endothelial cell’s proliferation resulting a narrow vessel lumen and consequently lead to impaired blood perfusion (Vijakumaran et al, 2021). This is the physiologically healing response to the injury of the innermost (i.e., tunica intima) blood vessel wall made of endothelial cells (Déglise et al, 2023).
- Hemihyperplasia is an abnormality having extra growth of any body part irrespective of normal body symmetry (Priyamvada et al, 2014). In most cases, asymmetric limb overgrowth occurred. Hemihyperplasia is a heterogeneous group and consists of different types such as isolated Hemihyperplasia, Hemihyperplasia associated with different types of syndromes such as Klippel Trenaunay Weber, Ehlers-Danlos, Neurofibromatosis type1, Russell-Silver, Proteus syndrome, Beckwith-Wiedemann syndrome, etc. (Dalal et al, 2006; Heilstedt and Bacino, 2004).
- Sebaceous Hyperplasia. In sebaceous hyperplasia ,one or more tiny yellowish papular lesions with a central umbilication that appear often on the face of adult patients. Surgical treatment is generally suggested but chemotherapy like Isotretinoin is also an effective therapeutic agent (Tagliolatto et al, 2015).
- Cushing’s Disease. Cushing’s disease is due to benign monoclonal pituitary adenoma having overproduction of adrenocorticotropic hormone (Lonser et al, 2017).
Hypoplasia
Hypoplasia undesirably affects tissue development due to lacking cells (Kandola, 2020). It can occur in many parts of the body. Some recently reported examples.
- Cerebellar hypoplasia refers to the reduced volume of the cerebellum (part of the brain, located at the back side) having preserved shape (Accogli et al, 2021).
- Optic nerve hypoplasia. Small optic disc and associated with other neuron-associated developmental disorders (El-Dairi and House, 2019).
- Congenital adrenal hypoplasia. Cortical areas are absent and replaced by large vacuolated cells in the adrenal cortex (Ouyang et al, 2021)
- Pulmonary hypoplasia. In pulmonary hypoplasia, incomplete lung development occurs (Tisekar and AK, 2022).
- Single bone hypoplasia is a rare condition of either isolated or multiple limb deficiencies. (Jain and Grewal, 2021).
Aplasia vs Hypoplasia
Hypoplasia is the underdeveloped condition of body organ. In contrast, aplasia is the complete absence of a body organ (Kandola, 2020).
Dysplasia
“Dys” means bad/abnormal, and “plasia” means growth. Dysplasia is the increase in the number of immature cells in a specific tissue. These cells lose the normal process of maturation and stratification (Rastogi et al, 2013).
Dysplasia vs Hyperplasia
Both dysplasia and hyperplasia reflect the same cellular abnormality in the form of an increased number. However, both have the distinct feature of cell maturity. Hyperplasia is the proliferation of mature cells in a tissue, while dysplasia is the increased number of immature cells.
Dysplasia vs Metaplasia
Both cellular abnormalities require stimuli-mediated transformation. External stimuli-mediated transformation leads to metaplasia. On the hand, internal stimuli-mediated transformation triggers production of dysplasia abnormality (GentleCure, 2021).
Dysplasia vs Cancer
Similarly, to cancer cells, dysplasia-associated tissues also have immature cells. But in contrast to cancer cells, dysplasia immaturity is reversible.
Types of Dysplasia
Based on microscopic observation, dysplasia may be mild, moderate, and severe (NCI Dictionary of Cancer Terms, n.d.).
Irreversible Type of Abnormal Cells
Several mutations in genes, (responsible for cell cycle, apoptosis, DNA repair/damage mechanisms, etc.) accumulate in the genome of abnormal cells. Cell proliferation fix these mutations in coming generations. Consequently, repairing mechanism unable cells to repair mutated cells. Mutation in cell cycle controlling genes, lead to uncontrolled growth of these cells. Moreover, these cells acquire immortality because apoptotic proteins (due to mutations) become unable to initiate programmed cells death mechanism. Such type of cells is classified as “Irreversible Type of Abnormal Cells” or in other words, “Cancer Cells”. These cells accumulate in the form of three types of tumors such as Benign, Premalignant, and Malignant tumors.
Benign Tumors
Benign tumor cells consist of less mutations as compared to malignant cells. Morphologically resemble with normal cells. Their growth rate is slow and strictly bound to their own tumor (Patel, 2020). These tumors have noncancerous cells.
Premalignant Tumors
Premalignant tumors consist of noncancers cells, but they can potentially decide to initiate malignant tumors. In other word premalignant are “potentially malignant” tumors (Brazier et al, 2022).
Malignant Tumor Cells
Malignant cells consist of more mutations as compared to benign tumor. These cells look like dedifferentiated cells, grow rapidly, and spread to other parts of the body (Devlin et al, 2021). These are cancer cells.
Classification of Abnormal Cells
| Type | Sub-Type / Criteria | Description | Examples |
| Reversible Abnormal Cells | Based on Size | ||
| Atrophy | Decrease in cell size due to loss of cytoplasmic proteins, organelles, or content. Leads to shrinkage of tissues. | – Muscle atrophy (due to inactivity, aging, or disease like cancer or diabetes) – Brain atrophy (in neurodegenerative disorders) – Testicular atrophy(from hormonal imbalance) | |
| Hypertrophy | Increase in cell size and volume due to enhanced workload or anabolic signaling. | – Cardiac hypertrophy(due to hypertension) – Skeletal muscle hypertrophy (due to exercise) – Smooth muscle hypertrophy (in uterus during pregnancy) | |
| Based on Number | |||
| Hyperplasia | Increased number of cells in tissue; morphologically cells appear normal. | – Benign Prostatic Hyperplasia (BPH) – Endometrial Hyperplasia – Sebaceous Hyperplasia | |
| Hypoplasia | Underdevelopment of tissues/organs due to fewer cell numbers. | – Cerebellar Hypoplasia – Optic Nerve Hypoplasia – Pulmonary Hypoplasia | |
| Aplasia (in contrast to Hypoplasia) | Complete absence of organ/tissue development. | – Aplastic anemia(absence of blood cell formation in bone marrow) – Renal aplasia(missing kidney) – Thymic aplasia (seen in DiGeorge syndrome) | |
| Based on Cell Differentiation/Organization | |||
| Dysplasia | Abnormal increase in number of immature cells in tissue, losing structural arrangement and maturation. | – Cervical dysplasia – Bronchial epithelial dysplasia (due to smoking) – Esophageal dysplasia | |
| Metaplasia (comparison only) | Change in cell type due to external stimuli, often reversible, differs from dysplasia which is due to internal stimuli. | – Squamous metaplasia of respiratory epithelium – Barrett’s esophagus – Osseous metaplasia | |
| Irreversible Abnormal Cells | Cancerous Cells | Caused by accumulation of genetic mutations in genes responsible for cell cycle, apoptosis, DNA repair. Lead to uncontrolled growth and potential immortality. | |
| Benign Tumors | Non-cancerous, slow-growing, morphologically resemble normal cells, remain localized. | – Uterine fibroids – Lipomas – Adenomas | |
| Premalignant Tumors | Non-cancerous but possess potential to transform into cancer. | – Actinic keratosis(precursor to squamous cell carcinoma) – Cervical intraepithelial neoplasia (CIN) – Colorectal adenomatous polyps | |
| Malignant Tumors | Cancerous cells, high mutation load, dedifferentiated morphology, fast growth, and invasive/metastatic behavior. | – Lung carcinoma – Breast cancer – Glioblastoma multiforme |
References:
- Accogli, A, Addour-Boudrahem, N, and Srour, M 2021 Diagnostic Approach to Cerebellar Hypoplasia. Cerebellum. DOI: https://doi.org/10.1007/s12311-020-01224-5
- Bonaldo, P and Sandri, M 2013 Cellular and molecular mechanisms of muscle atrophy. DMM Disease Models and Mechanisms. DOI: https://doi.org/10.1242/dmm.010389
- Brazier, Y, Rush, T, and Selchick, F 2022 Tumors: Benign, Premalignant and Malignant. MNT Knowledge Center.
- Dalal, A B, Phadke, S R, Pradhan, M, and Sharda, S 2006 Hemihyperplasia syndromes. Indian Journal of Pediatrics. DOI: https://doi.org/10.1007/BF02759927
- Déglise, S, Bechelli, C, and Allagnat, F 2023 Vascular smooth muscle cells in intimal hyperplasia, an update. Frontiers in Physiology. DOI: https://doi.org/10.3389/fphys.2022.1081881
- Devlin, C M, Simms, M S, and Maitland, N J 2021 Benign prostatic hyperplasia – what do we know? BJU International. DOI: https://doi.org/10.1111/bju.15229
- El-Dairi, M and House, R J 2019 Optic nerve hypoplasia. In: Handbook of Pediatric Retinal OCT and the Eye-Brain Connection. DOI: https://doi.org/10.1016/B978-0-323-60984-5.00062-7
- GentleCure 2021 Metaplasia vs. Dysplasia︱GentleCure. GentleCure. Available at https://www.gentlecure.com/metaplasia-vs-dysplasia [Last accessed 13 April 2023].
- Giroux, V and Rustgi, A K 2017 Metaplasia: Tissue injury adaptation and a precursor to the dysplasia-cancer sequence. Nature Reviews Cancer. DOI: https://doi.org/10.1038/nrc.2017.68
- Heilstedt, H A and Bacino, C A 2004 A case of familial isolated hemihyperplasia. BMC Medical Genetics. DOI: https://doi.org/10.1186/1471-2350-5-1
- Jain, A and Grewal, M 2021 Antenatal Single Bone Hypoplasia. Perinatology.
- Jopling, C, Boue, S, and Belmonte, J C I 2011 Dedifferentiation, transdifferentiation and reprogramming: Three routes to regeneration. Nature Reviews Molecular Cell Biology. DOI: https://doi.org/10.1038/nrm3043
- Kandola, A 2020 What to know about hypoplasia. Medical News Today. Available at https://www.medicalnewstoday.com/articles/hypoplasia [Last accessed 13 April 2023].
- Lonser, R R, Nieman, L, and Oldfield, E H 2017 Cushing’s disease: Pathobiology, diagnosis, and management. Journal of Neurosurgery. DOI: https://doi.org/10.3171/2016.1.JNS152119
- NCI Dictionary of Cancer Terms n.d. National Cancer Institute. Available at https://www.cancer.gov/publications/dictionaries/cancer-terms/def/dysplasia [Last accessed 13 April 2023].
- Nees, L K, Heublein, S, Steinmacher, S, Juhasz-Böss, I, Brucker, S, Tempfer, C B, and Wallwiener, M 2022 Endometrial hyperplasia as a risk factor of endometrial cancer. Archives of Gynecology and Obstetrics. DOI: https://doi.org/10.1007/s00404-021-06380-5
- Ouyang, H, Chen, B, Wu, N, Li, L, Du, R, Qian, M, Yu, W, He, Y, and Liu, X 2021 X-linked congenital adrenal hypoplasia: a case presentation. BMC Endocrine Disorders. DOI: https://doi.org/10.1186/s12902-021-00785-8
- Patel, A 2020 Benign vs Malignant Tumors. JAMA Oncology. DOI: https://doi.org/10.1001/jamaoncol.2020.2592
- Priyamvada, P S, Parameswaran, S, Sandeep, M, Shankar, V, and Swaminathan, R P 2014 Medullary sponge kidney and isolated hemihyperplasia. Indian Journal of Nephrology. DOI: https://doi.org/10.4103/0971-4065.133013
- Rastogi, V, Puri, N, Mishra, S, Arora, S, Kaur, G, and Yadav, L 2013 An Insight to Oral Epithelial Dysplasia. International Journal of Head and Neck Surgery. DOI: https://doi.org/10.5005/jp-journals-10001-1144
- Sartori, R, Romanello, V, and Sandri, M 2021 Mechanisms of muscle atrophy and hypertrophy: implications in health and disease. Nature Communications. DOI: https://doi.org/10.1038/s41467-020-20123-1
- Slack, J M W 2007 Metaplasia and transdifferentiation: From pure biology to the clinic. Nature Reviews Molecular Cell Biology. DOI: https://doi.org/10.1038/nrm2146
- Slack, J M W and Tosh, D 2001 Transdifferentiation and metaplasia – Switching cell types. Current Opinion in Genetics and Development. DOI: https://doi.org/10.1016/S0959-437X(00)00236-7
- Tagliolatto, S, Santos Neto, O de O, Alchorne, M M de A, and Enokihara, M Y 2015 Sebaceous hyperplasia: Systemic treatment with isotretinoin. Anais Brasileiros de Dermatologia. DOI: https://doi.org/10.1590/abd1806-4841.20153192
- Tisekar, O R and AK, A K 2022 Hypoplastic Lung Disease. StatPearls.
- Vijakumaran, U, Yazid, M D, Hj Idrus, R B, Abdul Rahman, M R, and Sulaiman, N 2021 Molecular Action of Hydroxytyrosol in Attenuation of Intimal Hyperplasia: A Scoping Review. Frontiers in Pharmacology. DOI: https://doi.org/10.3389/fphar.2021.663266
- Yuan, L, Zhang, Y, Wang, Y, Cong, W, and Wu, M 2012 Reactive lymphoid hyperplasia of the liver: A clinicopathological study of 7 cases. HPB Surgery. DOI: https://doi.org/10.1155/2012/357694



Interesting information